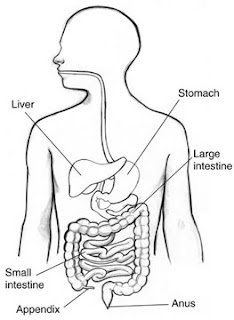
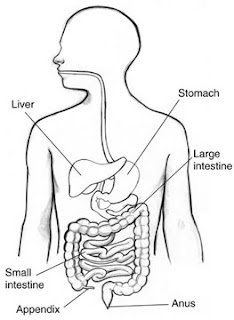
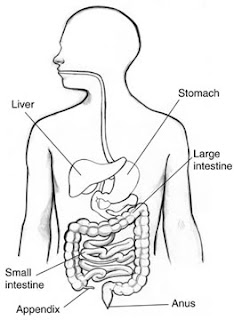
The stomach is a j-shaped, hollow, distensible organ located in the upper left corner of the abdomen. The stomach has several digestive glands, which produce stomach acid and enzyme that digest protein.
Common Stomach Diseases or Disorders
 Cyclic Vomiting Syndrome (CVS)
Cyclic Vomiting Syndrome (CVS)
CVS is characterized by episodes or cycles of severe nausea and vomiting that last for hours, or even days, that alternate with intervals with no symptoms. Although originally thought to be a pediatric disease, CVS occurs in all age groups. Medical researchers believe CVS and migraine headaches are related.
Many people can identify a specific condition or event that triggered an episode, such as an infection. Common triggers in children include emotional stress and excitement. Anxiety and panic attacks are more common triggers in adults. Colds, allergies, sinus problems, and the flu can also set off episodes in some people.
Other reported triggers include eating certain foods such as chocolate or cheese, eating too much, or eating just before going to bed. Hot weather, physical exhaustion, menstruation, and motion sickness can also trigger episodes.
Gastroparesis
Gastroparesis, is a disorder in which the stomach takes too long to empty its contents. It is also known as delayed gastric emptying. Normally, the stomach contracts to move food down into the small intestine for digestion. The vagus nerve controls the movement of food from the stomach through the digestive tract. Gastroparesis occurs when the vagus nerve is damaged and the muscles of the stomach and intestines do not work normally. Food then moves slowly or stops moving through the digestive tract.
Gastroparesis may occur in people with type 1 diabetes or type 2 diabetes. The vagus nerve becomes damaged after years of high blood glucose, resulting in gastroparesis. In turn, gastroparesis contributes to poor blood glucose control.
Symptoms of gastroparesis include early fullness, abdominal pain, stomach spasms, heartburn, nausea, vomiting, bloating, gastroesophageal reflux, lack of appetite, and weight loss.
Gastritis
Gastritis is not a single disease, but several different conditions that all have inflammation of the stomach lining. Gastritis can be caused by drinking too much alcohol, prolonged use of nonsteroidal anti-inflammatory drugs (NSAIDs) such as aspirin or ibuprofen, or infection with bacteria such as Helicobacter pylori (H. pylori). Sometimes gastritis develops after major surgery, traumatic injury, burns, or severe infections. Certain diseases, such as pernicious anemia, autoimmune disorders, and chronic bile reflux, can cause gastritis as well.
The most common symptoms are abdominal upset or pain. Other symptoms are belching, abdominal bloating, nausea, and vomiting or a feeling of fullness or of burning in the upper abdomen. Blood in your vomit or black stools may be a sign of bleeding in the stomach, which may indicate a serious problem requiring immediate medical attention.
Peptic Ulcers
A peptic ulcer is a sore on the lining of the stomach or duodenum, which is the beginning of the small intestine. Peptic ulcers are common: One in 10 Americans develops an ulcer at some time in his or her life. One cause of peptic ulcer is bacterial infection, but some ulcers are caused by long-term use of nonsteroidal anti-inflammatory agents (NSAIDs), like aspirin and ibuprofen. In a few cases, cancerous tumors in the stomach or pancreas can cause ulcers. Peptic ulcers are not caused by stress or eating spicy food, but these can make ulcers worse.
The most common symptom of peptic ulcer is abdominal discomfort. Other symptoms may include weight loss, poor appetite, bloating, burping, nausea, and vomiting. Some people experience only very mild symptoms or none at all.
Indigestion
Indigestion, also known as dyspepsia, is a term used to describe one or more symptoms including a feeling of fullness during a meal, uncomfortable fullness after a meal, and burning or pain in the upper abdomen.
Most people with indigestion experience more than one of the following symptoms:
The person feels overly full soon after the meal starts and cannot finish the meal.
The person feels overly full after a meal—it may feel like the food is staying in the stomach too long.
The epigastric area is between the lower end of the chest bone and the navel. The person may experience epigastric pain ranging from mild to severe.
The person feels an unpleasant sensation of heat in the epigastric area.
Other, less frequent symptoms that may occur with indigestion are nausea and bloating—an unpleasant tightness in the stomach. Nausea and bloating could be due to causes other than indigestion.
Rapid Gastric Emptying
Rapid gastric emptying, also called dumping syndrome, occurs when undigested food empties too quickly into the small intestine.
Early rapid gastric emptying begins either during or right after a meal. Symptoms include nausea, vomiting, bloating, cramping, diarrhea, dizziness, and fatigue. Late rapid gastric emptying occurs 1 to 3 hours after eating. Symptoms include hypoglycemia, also called low blood sugar; weakness; sweating; and dizziness. Experiencing both forms of gastric emptying is not uncommon.
Rare Stomach Disorder
Zollinger-Ellison syndrome (ZES)
ZES is a rare disorder characterized by one or more tumors in the pancreas, duodenum, or both. The tumors cause the stomach to make too much acid, leading to peptic ulcers in the duodenum. The tumors are sometimes cancerous and spread to other areas of the body.
Symptoms of Zollinger-Ellison Syndrome are similar to those of peptic ulcers and include burning abdominal pain, nausea and vomiting, weight loss, diarrhea, severe gastroesophageal reflux—a condition where gastric acid and food from the stomach backs up into the esophagus.
Suggested Reading:
View all Digestive Diseases Topics
Information courtesy of the National Digestive Diseases Information Clearinghouse (NDDIC), a service of the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK).
Page Last Revised: December 4, 2010
[Top of Page]
 The bacteria in the appendix can multiply and cause inflammation of the appendix. Symptoms of disease include pain in the lower right part of the abdomen, low-grade fever, nausea and vomiting.
The bacteria in the appendix can multiply and cause inflammation of the appendix. Symptoms of disease include pain in the lower right part of the abdomen, low-grade fever, nausea and vomiting. In a male fetus, the spermatic cord and both testicles—starting from an intra-abdominal location—normally descend through the inguinal canal into the scrotum, the sac that holds the testicles. Sometimes the entrance of the inguinal canal at the inguinal ring does not close as it should just after birth, leaving a weakness in the abdominal wall. Fat or part of the small intestine slides through the weakness into the inguinal canal, causing a hernia.
In a male fetus, the spermatic cord and both testicles—starting from an intra-abdominal location—normally descend through the inguinal canal into the scrotum, the sac that holds the testicles. Sometimes the entrance of the inguinal canal at the inguinal ring does not close as it should just after birth, leaving a weakness in the abdominal wall. Fat or part of the small intestine slides through the weakness into the inguinal canal, causing a hernia.